
Health


Allergies
Anemia

Anger

Anxiety

Asthma

Athlete's Foot

Back Pain

Bacterial Vaginosis

Bad Luck

Blisters

Bloodshot Eyes

Boils

Bronchitis

Bunions

Bursitis

Canker Sores

Cat Allergies

Cavities

Chapped Lips

Chest Congestion

Chills

Cholesterol

Chub Rub

Cold Sores

Common Cold

Constipation

Corns

Coughing

Cradle Cap

Cystitis

Cysts

Dandruff

Dehydration

Depression

Diabetes

Diaper Rash

Diarrhea

Dizziness

Dog Allergies

Ear Infection

Earaches

Eczema

Fatigue

Fever

Fibromyalgia

Flu

Gas
Germs in Air

Gingivitis

Gout

Hangovers

Hay Fever
Heartburn

Heat Rash

Hemorrhoids

Hiccup

High Blood Pressure

Hives

Hookworms

HPV

Iliotibial Band Syndrome

Indigestion

Insomnia

Irritable Bowel Syndrome

Jealousy

Jet Lag
Jock Itch

Kidney Stones

Lactic Acid

Lactose Intolerance
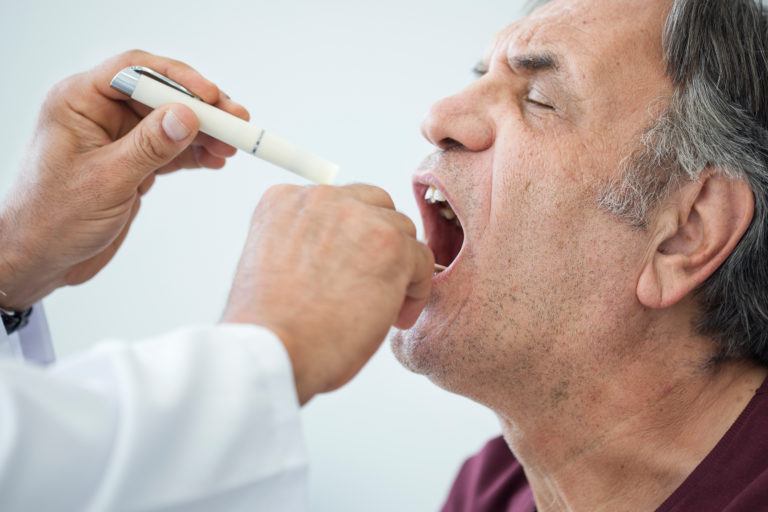
Laryngitis

Lazy Eye

Lice

Lisps

Loneliness

Malaria

Menstrual Cramps

Migraine

Mono

Morning Sickness

Mucus

Muscle Cramp

Muscle Knot

Muscle Stiffness

Nasal Congestion

Nausea

Negative Energy

Nits

Panic Attacks

Periodontitis

Periods

Phlegm

Phobia

Phone Anxiety
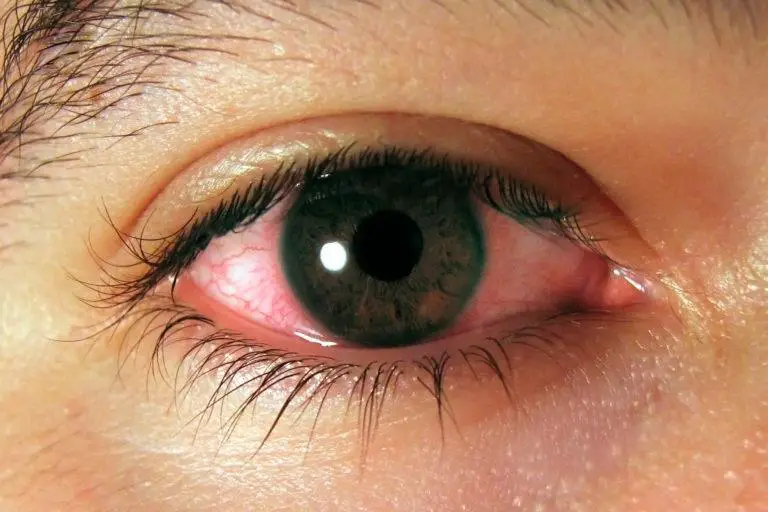
Pink Eye

Pinworms

Plantar Fasciitis

Plantar Warts

Plaque

PMS

Poison Ivy Rash

Poison Oak Rash

Postnasal Drip

Psoriasis

Puffy Eyes

Rashes

Ringworm

Rosacea

Roundworms

Scabies

Scabs

Seasonal Affective Disorder

Sensitive Skin

Sensitive Teeth

Shin Splints

Shingles

Sinus Headache

Sinus Infection

Skin Fungus

Sleep Apnea Syndrome

Smoking

Snoring

Sore Throat

Sores
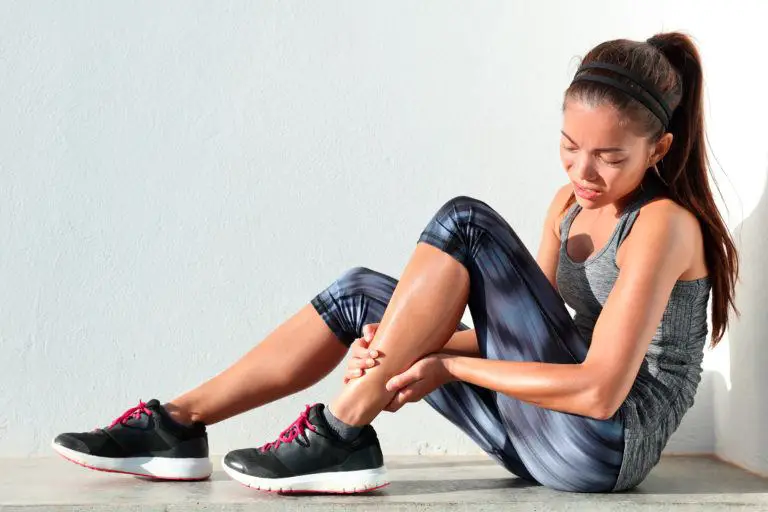
Sprains and Strains

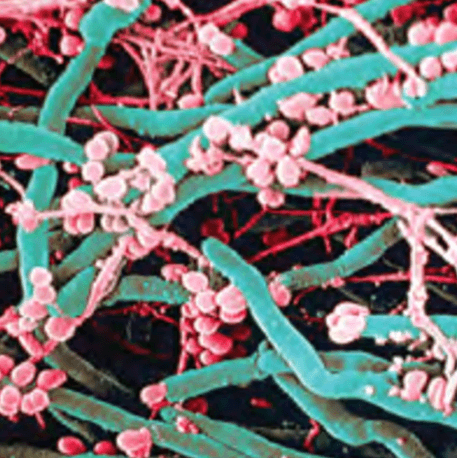
Staph Infection

Stomach Aches

Stomach Flu

Strep Throat

Stress

Stress Fracture

Stuffy Nose

Stye

Sunburn

Swelling
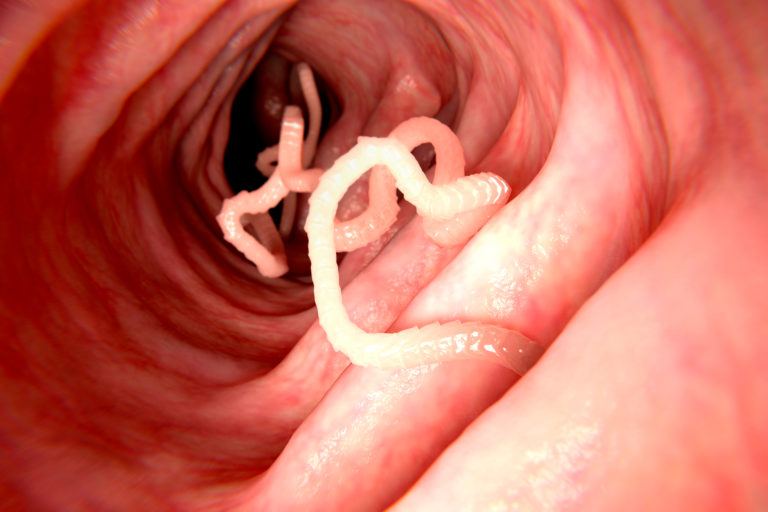
Tapeworms

Tendinitis

Tennis Elbow

Thrush

Toenail Fungus

Tonsil Stones

Toothache

Traveler's Diarrhea

Ulcers

Unwanted Pregnancy

Urinary Tract Infection

Vaginal Odor

Vaginitis

Vitiligo

Warts

Water Retention

Water Weight
